The inception of the Nurse Practitioner started in 1965 by a nurse and physician duo, but nurses have been serving in expanded roles, much longer than that.
In 1893 in the Lower East Side of Manhattan, where rapid industrialization and immigration created a huge need for medical and nursing care. Lillian Wald, a young graduate from the New York Training School, started the Henry Street Settlement (HHS). These visiting nurses would carry black bags with medications, home remedies, sterilized milk, ice, and other needs for the families they served. HHS also provided a savings bank, a library, vocational training, and social activities.

In 1903, nurses dispensing practices as well as what constituted practicing medicine were questioned after the passage of the Nursing Registration Act. “Nothing contained in this act shall be considered, as conferring any authority to practice medicine, or to undertake the treatment or cure of disease” (Article XII, 1903). At the turn of the twentieth century, the FDA required disclosure of certain ingredients such as alcohol, cocaine, chloroform, marijuana, and more. With the creation of new treatments and interventions, and federal and state legislative acts being created and changed almost daily, nursing, medicine, and pharmacy practice boundaries were constantly shifting.
Other nurses were creating similar public health services in other major cities like Boston, Philadelphia, and Chicago. There was the creation of the Frontier Nursing Service (FNS) in 1925 by Mary Breckinridge, a nurse midwife from a prominent Kentucky family. The FNS served the population in the Appalachian Mountains which was considered one of the most remote and difficult to reach populations. Nurses covered over 700 square miles of terrain by 1930, on horseback, and for the most part worked alone without any physician supervision.

The FNS as well as the Henry Street Settlement created committees to help navigate the changing legislative landscape to continue to be able to deliver treatment to their patients. By creating advisory committees and standing medical orders and guidelines for the nurses, they were able to oversee the welfare of the patients. These nurses were working to the fullest extent of their training.
Around 1950, most nurses were in hospitals where medical and nursing boundaries were more clearly defined. This was in great contradiction to those lone rangers of the Frontier Nursing Service, and other similar rural working nurses. In 1955 the American Nurses Association developed a model of nursing that would constrain nursing practice and lead to interprofessional conflict among nurses and physicians for the next several decades.
“The practice of professional nursing means the performance for compensation of any act in the observation, care and counsel of the ill . . . or in the maintenance of health or prevention of illness . . . or the administration of medications and treatments as prescribed by a licensed physician . . . The foregoing shall not be deemed to include acts of diagnosis or prescription of therapeutic or corrective measures.” (ANA, 1955, p. 1474)
Then, in 1965, nurse Loretta Ford, Ph.D. and Henry Silver, MD saw the need to bridge the gap in the health care needs of children and families in rural Colorado communities. Dr. Ford and Dr. Silver created a training program for nurses to give them advanced practice skills to be able to go into rural communities where most physicians would not go, and care for the communities there. This became the first Nurse Practitioner program.

Pictured above. Loretta Ford, Ph.D., who served as a nurse in the U.S. Army after her fiancé was killed in World War II. She was also honored this year during a ceremony for National Nurse Practitioners week, Dr. Ford, who will turn 103 years old this December is considered “the Mother of Nurse Practitioners”.
Despite the considerable resistance and criticism by some in the medical community, Dr. Ford and Dr. Silver successfully launched their Pediatric Nurse Practitioner program, which was then followed by Nurse Practitioner programs in Boston a few years later. By the 1970s there were more than 65 Nurse Practitioner programs in the United States. The American Nurses Association then starts to create a council on Nurse Practitioners to help legitimize the role, in part reversing its stance from the 1950s. In the 1985 the American Academy of Nurse Practitioners, which later became the American Association of Nurse Practitioners was established, creating more standards for credentialing, research, and advocacy. By 2023 there are more than 255,000 Nurse Practitioners in the United States! Dr. Loretta Ford was honored this year by the American Association for Nurse Practitioners.
Dr. Ford notes that Nurse Practitioners were intended to work independently. “A lot of them were doing it anyway. Now this has legitimized it,” Ford said. “We were the ‘Lone Rangers.’ We had to make decisions”. However, as it stands today, Nurse Practitioners are not able to work autonomously, in every state.
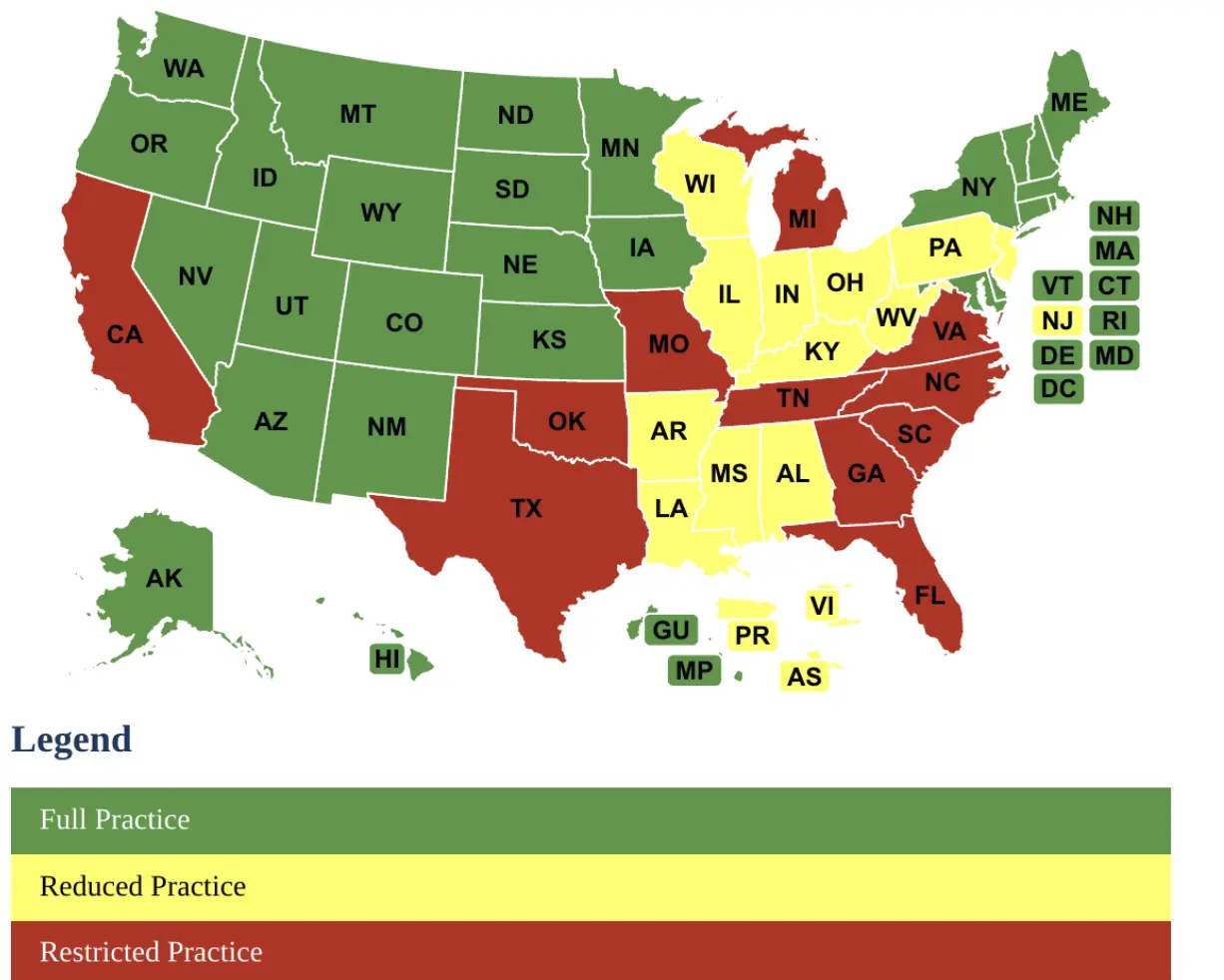
AANPs State of Practice Map: Shows which states are fully independent practice, reduced, or restricted practice states. No matter which state nurse practitioners live in, their educational standards, and credentialing remain standard. This means that in many states, Nurse Practitioners can’t practice to the level of their training and education. States that don’t have full practice tend to have larger costs associated with health care, larger discrepancies in healthcare in rural areas, and larger shortages of primary and mental health care.
Nurse Practitioners are educated, trained, and certified to work autonomously. Professional licensure already manages professions where there is overlap. Think of Osteopathic medicine, physical therapy, massage therapists, podiatrists, etc… All those professions have different educational pathways, and all have some overlap, but also offer distinct therapies to offer patients. None of those professions have oversight over each other. An osteopathic doctor doesn’t oversee a chiropractor, a podiatrist, or a massage therapist. Each profession has undergone training, certification and licensure in their area of expertise, none of them are practicing out of their own scope, but there are some overlaps in practice.
We still have significant healthcare shortages in many areas of the country. Nurse Practitioners are part of the healthcare team. Nurse Practitioners have been in the trenches, reservations, ghettos, mountains, on horseback in the snow to serve and care for people. Nurse Practitioners (and Registered Nurses) were also the ones still in the hospitals during COVID-19, when many physicians were at home.
Nurse Practitioners advocate for patients, advocate for quality care, accessible care, and affordable care. Celebrate this Nurse Practitioner week by advocating for those you advocate for you, your family, your friends. Advocate for Nurse Practitioners in your state to practice to the extent of their education, training and licensure. Contact your state representative, and state nurse practitioner professional advocacy centers. When you advocate for Nurse Practitioners, you are advocating for citizens to choose their healthcare.
Jaime Bristow, MSN, RN, BA, PMHNP-BC

Add a Comment